Exploring the Significance of Clinical Trial Patient Retention and Strategies for Improvement
Introduction
Patient enrollment is a significant and often limiting step in the initiation of a clinical trial, but patient retention (ensuring patients remain in the study after enrollment) is critical to the successful completion of a clinical trial. High patient dropout rates can severely impact the results of the trial, since it reduces the statistical power of the data.
In this article, we will discuss why patient retention is important and explain some proven methods for improving clinical trial patient retention.
What is patient retention in clinical trials?
Patient retention in clinical trials refers to keeping participants actively participating in the study through to its completion.
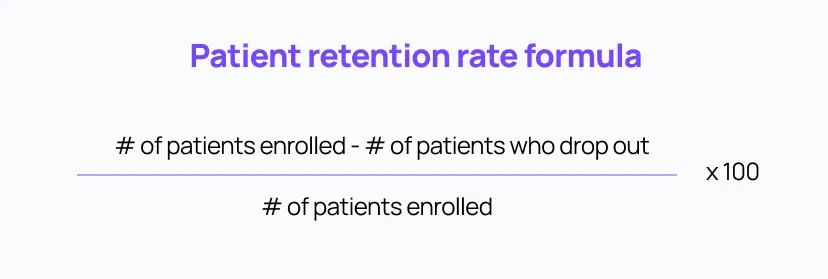
The patient retention rate can be calculated using the following formula:
Why is patient retention important in a clinical trial?
Patients leaving a clinical trial before its completion can cause the trial to run into major issues, since the statistical power of the results will be diminished due to having less valid data. If patients drop out early, it may cause (expensive) delays as sponsors try to recruit more patients to get back to the target sample size. If the final sample size is not large enough to draw any meaningful conclusions from the data, the trial may end up being stopped or canceled, representing a significant waste of invested money and time.
Understanding why patients choose to stay in a clinical study can help sponsors and investigators create the right patient retention strategies. In a 2021 study by the CISCRP, patients cited the following conditions/factors that would convince them to stay enrolled in a study (ranked in order of importance):
- Feeling or seeing direct benefit from the study drug
- Being informed of the clinical research progress on a regular basis
- Being offered flexible timing for study visits
- Having any out-of-pocket expenses reimbursed
- The ability to undergo study visits at home (i.e., remote study visits) rather than traveling to a study clinic
What are common motivations for participation in clinical trials?
Another important perspective to understand when designing clinical trial patient retention strategies is the reasons why participants may choose to enroll in clinical trials in the first place. Here are some of the common motivations for clinical trial participation:
- Finding an effective treatment: Many patients enroll in clinical trials to find a treatment for their condition, especially if the treatments currently available are not effective.
- Access to novel therapies: Clinical trials may provide an opportunity for patients to access the latest therapy or medication that is not available to the general public.
- Advancing science: Healthy participants enroll in clinical studies to contribute to the advancement of science and to help others. Helping others is also one of the common motivators for many participants suffering from disease or illness.
What are the main reasons why patients discontinue or drop out of clinical trials?
Here are some of the major reasons for patient dropouts:
- Financial burden: Taking part in a clinical trial could be financially straining for many participants since it could imply missed work, out-of-pocket travel costs, childcare services, and other related expenses. Many clinical trials require long-distance travel, which can be particularly challenging for elderly participants and those living in urban areas who may not be able to use more economical public transport methods.
- Scheduling inconveniences and family commitments: Patients may become overwhelmed by too many or too-frequent study visits. Since they have to invest significant time into the trial, it could further impact their personal or professional commitments. For instance, parents may have to arrange care for their children or elderly family members in order to attend the trial visits, which may be of significant duration when travel time is taken into consideration.
- Lack of engagement and understanding: Many participants struggle to understand the complex trial process and the terminology used in the clinical trial. A study conducted by CISCRP in 2013 found that the participants who struggled to understand the study scope were more likely to drop out than those who understood it.
- Stress and anxiety related to the trial: The same CISCRP report also found that one of the main reasons why many participants drop out early is due to anxiety and stress related to the trial sites and multiple visits. Participants who are less sociable and/or have lower self-confidence are more likely to drop out early. Such participants may have more difficulty (and thus lower motivation for) completing the study due to it being associated with experiences of severe stress and/or fear.
- Poor communication with the study center: Feeling informed, engaged, and valued throughout the clinical trial is important for patients, and lack of communication or poor communication with study staff and/or sites can lead to patients choosing to drop out.
How can clinical trial sponsors improve patient retention?
Understanding the common reasons many patients drop out of a trial can help you develop an effective clinical trial patient retention strategy. The overarching consideration for improving patient retention is reducing patient burden, which can be broken down into various aspects.
Reduce the burden associated with clinical trial participation
Patient burden may be best conceptualized by empathizing with their experience to imagine what participation implies for them, and then doing your best to honor their struggles and be considerate of their time. Adopting a patient-centric approach may be the single best way to encourage participants to complete the trial and help them feel involved and appreciated. Here are a few ways you can incorporate such considerations into the patient retention strategy:
1. Provide financial assistance
To ease the financial burden on patients, financial support can be offered during their participation in the clinical trial (understandably, this may not be feasible for some trials). Financial support would support participants in managing their financial responsibilities and worrying less about the costs associated with the trial.
Compensation could be simple (i.e., a lump sum for participation) or could be tied to specific expenses. For patients who have to travel long distances, compensation or discounts could be offered to assist with their travels to the study sites. Collaborating with travel and transportation agencies can help provide affordable options, reducing the stress of finding transportation and accommodation for the participants. Alternatively, transport could be pre-arranged for those who cannot afford or do not have access to other means.
2. Offer a flexible schedule
To accommodate patients’ other time commitments, a flexible schedule should be provided whenever possible. This can be achieved by offering multiple available time slots for appointments, or by allowing rescheduling of appointments if needed. By offering tailored support, participants can effectively manage their personal and professional schedules while participating in the trial. A great solution is to incorporate aspects of decentralization and enable some (if not all) visits to be conducted remotely (where possible), which could also make flexible scheduling more feasible.
3. Leverage technology where possible
Technologies can be leveraged to decentralize specific components of the trial, making the patient experience less burdensome and likely improving patient retention. For example, even simple things like phone call reminders can help patients with adherence to their medication dosing schedules and ensure that they are on track with protocol.
Decentralized data collection through methods like ePRO and eCOA can also reduce patient burden by reducing the need for frequent in-person visits to the study site. For example, patients can use wearable devices or smartphone apps to track their symptoms or specific health outcomes/endpoints, which can then be transmitted to the study team for monitoring, either automatically or by active data input by the participant.
4. Enhance understanding through education
Clear communication and accessible language should be used to educate patients and help them understand the scope of the study. All documentation should be written in simple language that clearly outlines the goals of the study as well as how participants actively contribute toward resolving the research questions. This will help patients feel engaged and understand how their active involvement represents a valuable contribution for the study and for clinical research in general, potentially increasing patient satisfaction and thus retention.
5. Reassure and engage participants
To reduce anxiety and prevent participant dropouts, it's essential to communicate effectively, identify concerns early, and provide support so patients can get answers to any questions they may have. By fostering open communication and a supportive environment, participants will feel more at ease, comfortable, and valued.
Conclusion
Clinical trial patient retention is one of the biggest issues that sponsors and study sites face. Aside from creating efficient and effective patient enrollment strategies, clinical trial sponsors must also consider tactics for maximizing patient retention and engagement. Putting the patient first and placing importance on their experience can improve patient satisfaction (and thus patient retention), reduce delays and losses, optimize clinical trial results, and even improve recruitment for future trials. Adopting a patient-centric approach is an optimal way to prevent dropouts and improve patient retention rates in clinical trials.