5 Simple Yet Highly Effective Patient Retention Strategies
Refresher: What is patient retention?
In clinical research, patient retention is the art of ensuring that participants who enroll in a trial remain in the trial until its completion. Here, we refer to patient retention as an art because although patients have full domain over their decision to remain or leave at any point throughout the duration of the trial, there are factors that the sponsor and study team can consider to make the trial more comfortable and enticing for patients to complete. These factors, which we have also described in detail in our article dedicated to explaining patient retention, include the design of the study protocol itself, interactions with the study team, and other aspects that tie in with the concept of patient centricity - empathizing with the patients’ journeys in order to minimize the burden the study places on them and optimize their experience.[1]
Why is patient retention so important?
Sample size is one of the fundamental factors of study design. Sample size is defined based on the number of participants and data points that will be required in order to make statistically sound conclusions that answer the research hypothesis, while also balancing ethical considerations, budget, and different study designs.[2] This includes consideration of how sample size will influence the two main types of error in clinical studies - type I error (treatment effect is identified when there was none; ‘false positive’) and type II error (treatment effect is not identified although one existed; ‘false negative’).[3] ‘Power’ refers to the ability of a study to correctly identify a treatment effect when one exists, and mathematically is the inverse of the risk of type II errors occurring.[3] A sufficient sample size is required in order to ensure study power. In general, larger sample size reduces sampling error and increases power. So, how does all this relate to retention?
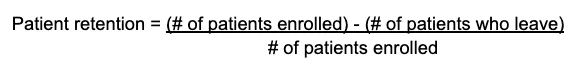
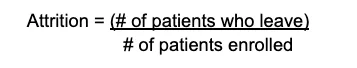
Patient retention is essentially the opposite of attrition, which refers to patients who are lost to follow-up due to various reasons, including deliberate drop-outs. We can use attrition to understand why patient retention is so important in clinical trials. Let’s say the study was designed such that 110 participants are needed for optimal power. If 3 participants leave the study, for whatever reason, then that represents a minor discrepancy and it is likely that the results will still be statistically meaningful. However, let’s say that 34 participants drop out - in this hypothetical case, this was because the study protocol demanded frequent visits during office hours, the treatment had difficult side effects, and the study lasted for more than 2 years - the high attrition rate of 30.9% (calculated as per the formula below) means that power is significantly reduced. Thus, it could be possible that the study treatment had a positive treatment outcome, but there are simply not enough data points at the end of the study to allow this outcome to be revealed. In other words, high attrition - low patient retention - presents risks to power and the validity of the study results.
Beyond issues related to power, poor patient retention represents significant monetary losses/waste, as it costs sponsors significant amounts of time and money to enroll each participant, raises ethical concerns, and may impact the reputation of clinical studies amongst the general population. So, it is clear that it is in the best interest of trial sponsors to expressly consider patient retention. Below we discuss 5 creative ways to increase patient satisfaction and optimize patient retention.
5 Simple, actionable clinical trial patient retention strategies
At the end of the day, it is impossible to completely control all factors that may cause patients to leave a study. In fact, trying to do so would likely incur efforts and costs that would not be justified by the marginal benefits. A better strategy is to identify (or predict) the main reasons why you may lose participants from a trial, and then to implement effective, practical, and measurable strategies to maximize the likelihood of patients sticking the trial through to the end. Here we present 5 simple, actionable patient retention strategies that you can incorporate into the respective aspects of your trial workflows. The overall focus is on creative ways to increase patient satisfaction and engagement – two main predictors of high retention rates.
1. Design patient-centric trial protocols
The trending concept of patient centricity keeps the patient’s lived experience at the forefront of the clinical trial design and operations. In the simplest terms, patient-centric trials put the patients first. In doing so, sponsors can make real efforts to minimize the burden the study places on participants, make their experience smoother and more enjoyable, and thereby increase the chances that participants remain in the trial through to its completion. So, what exactly makes a trial protocol patient-centric? The following list describes some principal ways to design trials that are more patient-focused and enticing.
Minimize unnecessary study visits and travel time - Can any of the study visits be omitted, combined, or conducted over the phone or through video calls? Can remote data collection tools like wearable devices be used to allow patients input data from home, or to collect health endpoint data automatically?
Collect only data that is necessary for the study results - While it may seem obvious, especially with new technologies it can be easy to get carried away and collect more and more data for the sake of it. Remember that each data point required by the protocol has the potential to place further responsibilities on the patients and incrementally increase the burden they experience.
Consider offering compensation for participants - Is it possible to remunerate patients for their time and commitment? Either for all participants, or based on individual travel distance/costs, etc.
Incorporate feedback - Successes and failures from past trials represent valuable insights into what works and what doesn’t work, and ideally would be used to consistently refine your trial designs and operations. Patient feedback is especially useful in this regard, as knowing what your patients found uncomfortable or burdensome can help you reduce that friction in future trials.
Keep the patient’s first-hand experience as the top priority - This is a bit of a circular definition, but it deserves repeating. If you want to try to grasp how patient-centric your trial is, visualize (or simulate) the patient’s journey, from consenting and enrollment through to follow-up. Note any visits or requirements that feel difficult and that could be made smoother through some aspect of intentional trial design.
Avoid too much complexity in protocols when it can be avoided - Patients who understand the protocol and what is expected of them are more likely to remain in the study. Further, the protocols should be manageable in the midst of a busy life, as participants have other commitments besides the trial. Consider the use of eConsent forms to ensure full comprehension of the protocol during onboarding, and simplify wherever possible!
Decentralization - Fully decentralized trials (DCTs) and hybrid (partially decentralized) trials leverage technology to enable patients to enter data remotely, attend study visits over the phone from the comfort of home, and minimize the number of in-person study visits. Besides the potentially significant benefits for patients in terms of reduced trial burden, decentralization offers many benefits to sponsors and sites as well, such as reducing site visits and in-person monitoring, removal of geographic barriers during enrollment, and enhanced data management and trial monitoring from a central location.
What might this look like in practice?
Hypothetical example: ABC BioPharma plans to investigate their new drug designed to lower blood pressure, LOWB. The preliminary protocol design involves 10 in-person study visits, wherein patients will have their blood pressure taken. A consultant points out that equipping all participants with a home blood pressure monitor would turn out to be 10% less expensive than contracting all 4 study sites to conduct those 10 study visits for each patient. So, ABC BioPharma decides to decentralize the trial, since in this case the health endpoint measured is simple and relatively easy to record at home. Each patient comes in for a first visit, wherein they are instructed on proper use of the blood pressure monitor. The patients record their blood pressure readings not only 10 times, but 30 times throughout the trial duration, since the measurement only takes 5 minutes. The patients feel at ease and engaged when inputting their data, without having to travel repeatedly to the nearest site for a simple procedure. Meanwhile, ABC BioPharma cut down on costs, offered an enhanced patient experience, and collected 3x more data points than originally planned (while still ensuring this was manageable for participants), giving them higher precision in determining when the effect of LOWB may begin to appear.
2. Treat patients with respect at every touchpoint
Generally, patients would like to feel that their contribution is valued, that their concerns are being heard, and that they are respected and seen. Patients are more likely to drop out of a study if they perceive that staff at study sites are unavailable, uninterested, or if they constantly see new faces at each visit.[4] This reveals the importance of interpersonal interactions in the patient’s experience. A simple way to approach this is to see each patient as a unique relationship that needs to be maintained. Every single interaction between site staff and the patient is an opportunity to make or break the relationship. If possible, schedule visits such that patients see the same study staff throughout the trial.
Staff and investigators could be given deliberate training on protocols related to treating patients with respect, in particular in relation to empathizing with their condition and the hardships they may be experiencing as a result of the trial and/or their underlying condition. In high-stress environments, patients may also feel more stressed, so it is important to be able to count on staff who can remain calm and professional in various situations.
Waiting times at study sites may play into this, as it is natural to feel disrespected or unseen when made to wait for a long time despite having an assigned appointment time. This adds another argument to the importance of selecting sites with efficient and well-managed operations. One idea is to assign a dedicated staff member to greet patients at study visits, helping the patient feel welcomed and adding a personal touch to their experience, further providing someone who can clearly communicate delays and also offer conversation to pass the time, if the patient so desires.
3. Establish personal, two-way communication
Tying in with the previous point, another way to increase engagement is to enhance communication between patients and the study team, which builds trust in the relationship. This not only helps patients recognize that their participation is valued and enhances their sense of engagement with the trial, but it is also useful for allowing them to voice concerns - and allowing the investigator/site staff to potentially address these concerns - before they make a one-sided decision to drop out/become unresponsive due to frustrations or minor issues that could potentially have been resolved with open communication.
We acknowledge that this could represent significant or unrealistic investments of time on the sponsor’s part, so the following strategies are chosen based on their simplicity, while still being effective for optimizing retention.
Make it clear that patient feedback is valued and welcomed - Provide simple ways for patients to provide feedback, ideally anonymously to make sure they feel comfortable being honest. Patient experience surveys can be distributed after the trial, but also interim to collect feedback on a rolling basis. At the same time, be mindful of overburdening them or wasting time/resources on too many communications that start to feel like spam. A follow-up survey of patient experience a few weeks or months after the end of the trial can be a good idea, as patients will likely have a more stable, emotionally grounded view of the experience as it becomes more distant. Design the main parts of feedback surveys as if they were CRFs - with clear, constrained fields - which will make it easy to analyze the responses and identify patterns. Nonetheless, a single free-text field for “additional concerns” would make it possible for patients to share anything else that wasn’t captured by the form.
Make staff available to answer questions or talk to patients - Consider both phone and online chat support, open as often as possible. This setup could be centralized so as to keep costs down, offering one help line with two team members for all patients across all sites, for example, or for every X number of patients in larger trials.
Set automatic reminders to help patients stay on track with their study visits, data entry times, surveys, etc. - make the reminders personal and interactive/engaging.
Follow-up quickly with unresponsive patients - By reaching out to patients who have missed even a single appointment or phone call, you can attempt to recapture their attention and commitment, or resolve any issues that may have led to the missed visit. This helps them recognize that you are taking their individual participation seriously and that they are important to the study, and can hopefully prevent some would-be drop-outs.
Pro tip: Have staff remember one personal fact about each patient - Full credit for this one goes to Weave.[5] Remembering even the most minor detail about a patient and being able to ask them about it can add a particularly personal touch to their visits, which will go a long way toward enhancing their satisfaction. Of course there are cases wherein this is simply impractical, but you could consider tricks like making a quick note on the patient’s file so that any staff member could see it and ask the patient a personal question or say something meaningful to them.
4. Increase engagement through educational material, updates, and interactive content
Clinical trials can offer a way for patients to take a more active part in their healthcare, but much of that will depend on the trial design and the intentions of the sponsor. The trial represents an opportunity for them to learn more about their condition, to become more familiar with clinical research and its value for society (and thus the value of their personal contribution), and to feel like an active member of the study and their own healthcare team.
In traditional site-based trials, patients often come in to study visits, have measurements taken, and go home. Are there ways that this routine can be spiced up to make the trial more engaging and enjoyable for them overall? Here are some ideas:
Share updates about the trial’s progress - Obviously these updates cannot reveal results or include sensitive information, but sharing progress updates can help patients remember that they are taking part in an active research project aiming to benefit the broader (and future) population. Updates could focus more on progress made than progress to be made, in order to boost the sense of optimism amongst patients. For example, celebrate the fact that 4 of 9 study visits have been completed smoothly, rather than the 5 that are left.
Publish educational material - Beyond the study background, objectives, and requirements laid out in promotional materials and consent forms, sponsors could share educational material to simply help the patients remain engaged and offer them learning opportunities. A bonus to this approach is that many materials could be reused between different studies. Keep in mind that the average person does not have high-level scientific/medical literacy - use simple language and explain concepts clearly without too much jargon. Topics could include:
- Biological details and underlying mechanisms of the condition being studied
- Advances and cutting-edge research on the condition
- The importance of clinical research in healthcare and the benefits of participation
- Advances in clinical research in a broader sense
Aim to make study materials interactive and engaging - Wherever possible, add interactive components to study materials to enhance patient engagement. Some ideas include:
- ePRO - Electronic patient-reported outcomes can be set up to let patients take their own basic physiological measurements, enter data themselves, report on their symptoms, etc. Wearable and connected devices are engaging and could even help some patients feel empowered.
- Interactive videos/images in eConsent can improve engagement and comprehension simultaneously - patients who clearly understand a study are less likely to leave it.[3]
- Gamified surveys and data collection - In some cases, surveying and data reporting tasks for patients could be made more “fun” while still remaining clear and serious. Perhaps a competition or incentive could be established, for example wherein all participants who complete 100% of study data collection surveys on time win a gift card to a nice restaurant, or are entered into a draw to win a larger prize. ePRO systems that run through apps could be gamified, awarding points each time a survey is completed on time, and showing a leaderboard of active participants. It is important not to go overboard and detract from the seriousness of the trial, but these small touches could sometimes go a long way toward enhancing a patient’s enjoyment of their trial participation.
5.Put yourself in the patient’s shoes: Predict stressors and minimize patient burden
A great way to get up close and personal with the patient experience is to simulate going through the entire trial. Go slowly and purposefully, step-by-step, from consenting through to follow-up activities. Use the actual study materials, calculate travel time and costs for an average distance from study sites, wear the connected devices, fill out the surveys, etc. Based on that experience, identify stress points, predict potentially problematic areas, and see if you can do something to eliminate or work around these points. Evidently, some will be unavoidable - in those cases, see if you can facilitate ways for these stressors to be minimized or addressed as quickly as possible. For example, in trials requiring necessary visits to sites, consider patients’ commutes to the study sites and how that may look for them - is there any way to make these trips smoother or less costly, such as pre-arranged taxis or financial compensation? Could an additional staff member be added to the support team in the period after visits involving difficult procedures? Is additional training on wearable devices necessary in order to avoid confusion/frustration and increased calls to the site for technical assistance?
Another great insight into patient experience comes from their feedback from prior studies. This ties into the idea of incorporating feedback right from the start, in the trial design phase.
6. Bonus tip: Oversample if high attrition rates are inevitable/predicted
The truth of the matter is that there are some studies that will inevitably require difficult tests/procedures, burdensome study visits to use specialized equipment, or wherein high death rates are likely due to the severity of the underlying condition being treated. If you have gone over these 5 patient retention strategies but still predict high dropout/attrition rates, then you can consider taking preemptive corrective action by slightly oversampling (over-enrolling).
The aim of oversampling is to ensure your study retains power even after a certain percentage of participants drop out. Consider looking at attrition rates for previous studies that are somehow related - perhaps trials for the same condition, or trials conducted at sites you’re using that involved similar patient demographics - and aim to offset those estimates by oversampling proportionately. Evidently, any potential benefit of oversampling can be easily negated by the increased costs and time required for enrolling additional participants, so aim to find a balance that works for your budget and trial timeline. For example, if your sites tend to experience 15% attrition rates for trials in a similar clinical area, enrolling an additional 50% over your target sample size may represent a significant expense that is not justifiable by the marginal benefit. On the other hand, under-enrolling or experiencing unexpectedly high attrition rates can invalidate the study results, which could represent an ever greater loss of funds. Again, aim to find the balance that works for your organization.
Conclusion
Along with enrollment, retention can represent a major challenge for some clinical trials and sites, with high attrition rates representing a cause of delays, monetary losses, underpowered studies, and ethical issues. Nonetheless, with the rise of patient centricity and a multitude of useful technologies, sponsors are better equipped than ever before to be aware of common issues leading to low retention rates and take steps to optimize patient retention. The various patient retention strategies discussed in this article should be a good starting point for integrating considerations of patient retention directly into the trial protocol, and in all of its operations. It is important to be proactive here, since although some degree of attrition is inevitable, with the right planning and attitude there is often a lot that can be done to encourage patients to remain in a trial through to its completion.
Beyond any individual study, boosting patient satisfaction makes waves throughout the industry - the general population becomes more comfortable with participation in clinical research as trials become more patient-centric and patient-friendly, enhancing recruitment efforts for future trials… and the positive feedback loop continues!