Clinical Trial Basics: Screen Failure
Screen failures can significantly increase the cost burden on both sponsors and sites, so it’s essential to understand why they arise and what can be done to minimize screen failure rate.
Subject screening definition
In clinical research, subject screening or patient screening is the process of reviewing a candidate against the inclusion and exclusion criteria of the trial to determine their eligibility. This includes recording demographic information and asking general health questions, but may also include physical exams, lab work, and diagnostics tests such as MRIs, CT scans, or x-rays. The latter screening processes are more invasive and can only start after a candidate gives their informed consent, whereas basic demographic details can be gathered prior to consenting.
Definition of screen failure in clinical trials
A candidate who undergoes screening - meaning they are checked for eligibility - but who does not meet the clinical trial's inclusion/exclusion criteria is referred to as a screen failure. The definition of screen failure also includes eligible candidates who give their informed consent but then:
- Withdraw their consent
- Suffer an adverse event and cannot participate
- Relocate
- Prove to be non-compliant
It’s difficult to obtain consistent statistics on the prevalence of screen failures because there is no standardized definition of a failed screening, meaning there is also no uniform protocol for reporting screen failures.
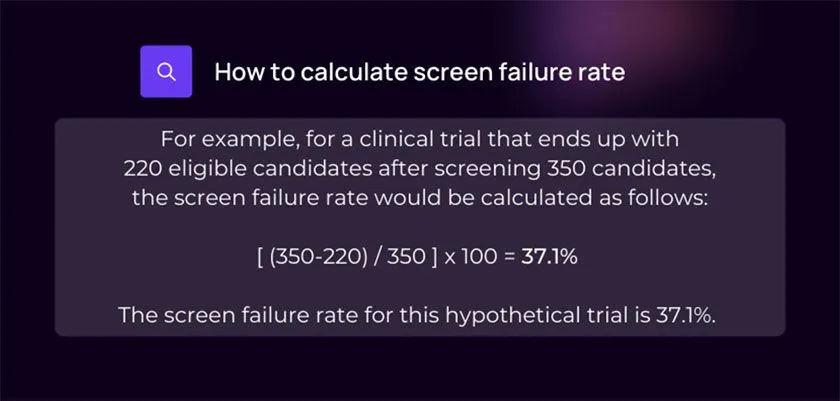
How do you calculate screen failure rate?
The screen failure rate formula takes the number of ineligible candidates divided by the number of screened candidates, and then multiplies that by 100 to get screen failure rate as a percentage:
Does screening occur before or after informed consent?
Most aspects of screening can only be performed after a candidate has given their informed consent. Any screening procedure or questioning that is considered to go beyond basic demographic factors, or that involves an intervention or invasive procedure, requires prior consent of the participant. For example, scans or laboratory tests cannot be performed prior to consenting.
However, clinical trial recruiters can pre-screen candidates against the trial’s inclusion and exclusion criteria based on basic information such as age, sex, current diagnosis, co-illnesses, and prior treatments the patient has undergone for their condition. Using this information, investigators can determine basic eligibility, and further screening procedures may be conducted after the patient is enrolled and consented.
How much does a screen failure cost sponsors?
Screen failures represent lost time and monetary resources, costing both sites and sponsors. The extent of loss is dependent upon how far along the screening process the failure occurs, which is why pre-screening (for example, by leveraging Power’s advanced pre-screening feature) is an important step.
The actual monetary cost of a screen failure is difficult to approximate, due to the high variability between studies. Factors that influence the cost of screen failures include the study protocol, the number of eligibility criteria and how narrow they are, and the specific screening processes employed. Screen failure costs can also vary amongst different therapeutic areas of clinical research; if expensive procedures are required to determine eligibility, each screen failure will represent a greater cost to the sponsor.
The fee arrangement between sponsors and sites, detailed in the clinical trial agreement (CTA), will determine who bears the costs of screen failures. It has been suggested that sponsors opt not to use a fixed cost per screening, as it may incentivize certain sites to screen candidates with low eligibility, increasing the screen failure rate.
A general guideline for reducing screen failures and associated costs is to use digital solutions for initial pre-screening and for informed consent.
What are the most common causes of screen failure?
The most common reason for screen failure is the candidate being ineligible for the trial, due to meeting exclusion criteria and/or not fulfilling inclusion criteria.
In other cases, a candidate may be deemed eligible but decide not to participate in the study, which could be for nearly innumerable possible reasons, such as lifestyle constraints, the duration of the trial, procedures involved, doubts and fears, opting for another treatment, or due to the potential adverse effects associated with the study drug. This is another reason why it is so vital to be transparent and detailed in all promotional material, such as recruitment flyers and online recruitment ads, so that participants have as much information as possible right from the start and can make an educated choice whether or not to proceed to screening.,
Another reason for an exaggerated screen failure rate is working with enrollment sites according to a flat-fee payment model wherein the site is paid for the total number of patients screens. This can result in indiscriminate screening of ineligible candidates and inflated screen failure rates.

5 ways to reduce screen failure rate
There are several methods that both sponsors and sites can utilize to reduce the screen failure rate in clinical trial recruitment. Check these five strategies and try them out in your next trial - mix and match and see what works best for you, and remember to monitor and track recruitment success so you can continue to make improvements.
1. Perform thorough pre-screening
Take full advantage of the pre-screening process to filter candidates before calling them to your site and getting the research team involved. Remember, the further along the recruitment pipeline the screen failure occurs, the more costly it’s likely to be. Look to digital solutions such as Power, where patients sign up for clinical trials that are a good fit, and fill out a pre-screener. The site receives patient referrals in real time complete with all pre-screening and demographic information.
2. Design patient-centric protocols
The more flexible the trial is for patients, and the more consideration that’s given to patient experience, the more willing participants will likely be to enroll in the trial. If a trial is sufficiently enticing - offering to fulfill the patient’s motivation for participating, without requiring an unmanageable burden - eligible candidates are more likely to decide to enroll. Focus on designing patient-centric trial protocols that prioritize their experience and support them to feel seen and valued as collaborators in the clinical research process..
3. Leverage decentralized technologies
Digitalizing and decentralizing your pre-screening and consenting processes (and even parts of screening) can help lower screen failure rate, or at least their costs. Technologies such as eConsent help engage and educate candidates more thoroughly, thus assisting them in making informed decisions and judging their own eligibility, without the costs of staffing site visits for each patient. For remote and decentralized clinical trials, eConsent also enables remote enrollment, further widening your potential trial population.
4. Monitor screen failures and quickly address any problems identified
Monitor your screen failure rate throughout the enrollment process, at each study site and overall. Aim to identify the causes, where possible, and act to rectify the issues leading to screen failures. For example, high pre-screen failures could highlight a lack of specificity in your clinical trial recruitment materials - swap-out content for another version with better transparency about the study protocol. High screen failures across all sites might indicate that your inclusion/exclusion criteria are overly restrictive - see if any eligibility criteria can be adapted, to open up access to wider populations without sacrificing the robustness of the study design.
5. Establish an appropriate fee structure for screening
To avoid the issue of sites screening indiscriminately to obtain a per-patient fixed screening fee, ensure you reach an appropriate fee structure agreement with your enrollment site(s). Consider a performance-based payment scheme, where sites are rewarded more for screenings that lead to consenting. Hash out the details and your expectations explicitly in the CTA, and make sure the fee structure works out for the trial site as well, as it’s important that they are motivated for the trial to succeed.
Conclusions
Screen failures are part of the clinical trial enrollment process and likely cannot be avoided completely. However, sponsors who are prepared with realistic expectations, well-designed patient-centric protocols, appropriate eligibility criteria, and who leverage digital technologies to their advantage can minimize screen failure costs and achieve recruitment success.